Nursing Annual Report 2024 | Sailing Towards Magnet Mastery
Empirical Quality Outcomes |

Nurse Driven Mobility Program: Johns Hopkins Mobility Program to Improve Patient Activities
Patients admitted to acute-care settings spend more than 50% of their time lying in bed. Prolonged bedrest for hospitalized patients places them at a higher risk of developing debilitating hospital-acquired conditions, including pressure injuries, pneumonia, and prolonged length of stay. Increasing mobility is important to hospitalized patients, improving respiration, preventing bed complications, and speeding recovery. El Camino Health adopted the Johns Hopkins Mobility Program, a nurse-driven early progressive mobility protocol. The Johns Hopkins Activity and Mobility program is an evidence-based activity program that promotes and maintains patient activities according to an assessed mobility goal.
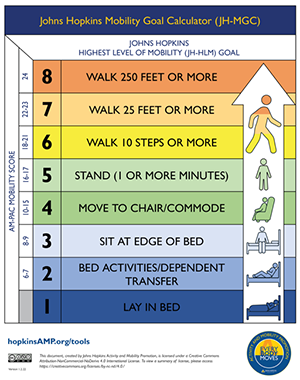
John Hopkins Mobility Goal Calculator
The goals of nurse-driven early mobility are to promote a multidisciplinary focus on early mobility as part of the daily clinical routines to maintain patients at their pre-hospital baseline mobility and functional levels as much as possible. A colorful wall mobility goal chart is posted in patients' rooms to encourage progressive mobility by showing their daily mobility goals and engaging them to participate in their progress.
The mobility program includes a multidisciplinary team of unit nurse managers, nurse educators, and frontline nursing staff identified as mobility advocates. Nurse managers monitor unit performance (e.g., percentage of patients meeting mobility goals), disseminate feedback regarding unit performance to unit staff, and identify and address unit-level barriers to meeting these goals. Nurse educators ensure that all staff, including new hires, complete the required Johns Hopkins mobility program training and provide training to address unit-level barriers to mobilizing patients. Frontline nursing staff selected as mobility advocates receive specialized training and serve as the respective units' experts.
A critical component of the Johns Hopkins Activity and Mobility program is measuring how patients meet their mobility goals. It provides insight into patients' mobility levels compared with their physical capacity and is reported for each hospital unit. These reports are built with patients stratified by the highest goal ranges (3-5, 6, and 7-8) to provide feedback on patient goal achievement among those with similar mobility levels. Since the adaptation of the program, we have seen an improvement in patients reaching their daily mobility goals, with an overall mobility goal achievement of 62%.
Improving Blood Transfusion Practices in a Medical-Surgical Oncology Unit: Poster presentation at ACNL (February 2023)
Edna Ogbonnaya, RN poster presentation at ACNL conference
The Medical Surgical Oncology team is one of the leading blood transfusion units in the organization. A significant focus was placed on improving safety measures, particularly by emphasizing the best practice of monitoring vital signs fifteen minutes after starting a blood transfusion, as this is the critical period for adverse reactions. Compliance rates for this metric rose from 84.5% in 2020 to an impressive 96.5% in 2023. This improvement followed the implementation of a quality improvement plan, which involved clarifying metric requirements, providing a user-friendly algorithm for nurses to reference, and ensuring contact reminders from the blood administration RN.
Collaborative Aid Through Listening & Motivation: CALM Team Pilot
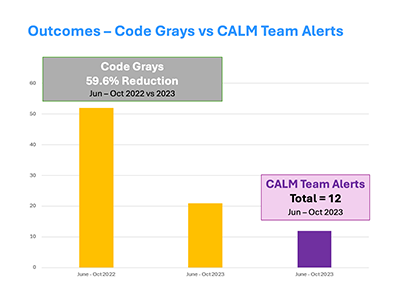
The Collaborative Aid Through Listening and Motivation, known as CALM, is a program comprised of Proactive Rounders and Responders for behavioral escalation. The program, which was piloted from June 2023 to October 2023, was modeled after similar response teams at the University of California in Davis (UC Davis) and the University of California in San Francisco (UCSF) but customized to El Camino Health (ECH).
The primary goals of CALM consist of patient safety, harm prevention, and early coordinated interventions for escalating behaviors. Training was provided to accomplish these goals. The ECH Nursing staff participated in prior training courses on Delirium and Dementia, as well as Diversity & Inclusion. In May 2023, healthcare professionals from our Mental Health & Addiction Services provided training to multidisciplinary staff on Motivational Interviewing & Trauma Informed Care. In total, over seventy-five multidisciplinary team members participated in the CALM Pilot.
On June 6, 2023, the CALM Pilot launched in 2C Medical and 3C Telemetry/ Stroke units. The CALM Team and nursing staff supported the patients with Broset risk for violence screenings, CALM Team Referral Lists & Alerts, de-escalation techniques, and debriefing skills. Overall, the CALM Pilot produced highly successful outcomes with a Code Gray Reduction Rate of 59.6% and 12 CALM alerts.
