By Andy S. Yu, M.D.
Dr. Yu received his M.D. degree from University of Chicago Pritzker's School of Medicine; internal medical residency training at UCLA Sepulveda Program; gastroenterology fellowship at UC Davis; general hepatology fellowship at University of Southern California; transplant hepatology fellowship at UCLA Cedars-Sinai Medical Center.
請點擊此轉換成中文
Among Asian American males and females alike, colorectal cancer is the 3rd most commonly diagnosed malignancy. Colorectal cancer is also the 3rd most common cause of cancer deaths. It contributes to approximately 50,000 deaths in the United States annually. Unfortunately, one-third of the U.S. general population above age 50 has never been screened for this life-threatening disease. Medical studies have recently revealed that there is an increasing trend for younger Americans to be affected by colorectal cancer. As of May 30, 2018, the American Cancer Society lowered the age threshold for colorectal cancer screening from 50 to 45 for average-risk individuals.
What is Colorectal Cancer?
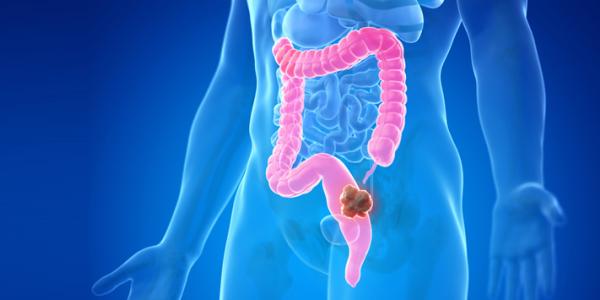
The large intestine is the lowest portion of the digestive tract. It starts with the colon, which is 4 to 6 feet in length, followed by a 6-inch long rectum, before transitioning into the anus. In other words, "large intestine" can be used interchangeably with "colorectum." The purpose of the colon is to absorb fluid, mineral, and nutrients. The rectum stores the feces until a convenient time for defecation.
Colorectal cancer occurs mostly on the inner lining, or mucosa, of the large intestine. Most colorectal cancers start from normal mucosal tissue and evolve through a benign and yet precancerous stage of adenomas due to a cascade of genetic mutations, before finally becoming actual malignant growths. The chances of harvesting colorectal adenomas approximate 30%, 50%, and 70% by ages 50, 60, and 70, respectively.
Staging Colorectal Cancer
Colorectal cancer must be confirmed by tissue diagnosis under the microscope, followed by imaging studies to assess the extent of the disease. The tumor is at Stage 0 if it remains limited to the surface lining of intestinal mucosa. Stages 1 and 2 characterize tumors that have invaded into but not extended beyond the intestinal wall. Stage 3 disease describes cancer spreading to lymph nodes or nearby organs. Stage 4 disease occurs when cancer cells have traveled to faraway organs, such as the lungs, liver, brain, or adrenal glands.
Clinical Signs and Symptoms of Colorectal Cancer
Colorectal cancer often remains clinically silent until advanced or late-stage disease has developed. Clinical manifestations may be divided into four categories.
Bleeding. There are different types of colorectal cancer bleeding. Brisk bleeding from a site closer to or in the rectum usually appears as bright red blood. On the other hand, relatively rapid bleeding from a site closer to the small intestine may appear as black and tarry stool. But when bleeding occurs at a very slow rate, anemia may evolve over time with initially no or minimal symptoms.
Change in Bowel Habits. Colorectal cancer may present as altered bowel habits, such as chronic intermittent diarrhea, constipation, or diarrhea alternating with constipation. A bulky tumor in the intestine may block the passage of large chunky stool but allow the flow of liquid substance.
Pain or bloating. Colorectal cancer may also manifest as abdominal pain or bloating. Surgical emergency, requiring immediate operation, occurs when an advanced tumor has blocked off part of the intestine, causing obstruction and dilation, threatening perforation.
Nonspecific Findings. The final category of clinical manifestations include more subtle or nonspecific findings, such as fatigue, weakness, weight loss, and wasting of the body, all of which may be associated with advanced colorectal cancer.
Younger patients, especially those under the age of 50, are more frequently affected by cancer in the distal or last part of the intestine. The presence of bright red blood from the rectum may incorrectly be attributed to hemorrhoids, which could delay the correct diagnosis.
Risk Factors for Colorectal Cancer
Genetic mutations are the most important and highest risk factor for colorectal cancer. Nevertheless, half of all colorectal cancer patients do not have positive family history. On the other hand, the risk is markedly increased by positive family history of 1st-degree relatives with either colorectal cancer or advanced-stage precancerous adenomas.
Moderate-degree risk factors include personal history of colorectal cancer, precancerous adenomas, or pelvic radiation therapy for prostate or ovarian cancers.
Colonoscopy is the Most Ideal Method to Diagnose Colorectal Cancer
Colonoscopy is the screening test of choice for colorectal cancer. As noted, the American Cancer Society recommends screening for colorectal cancer start at age 45 for all average-risk individuals, to detect adenomas before they become malignant. Besides colonoscopy every 10 years, other viable but less effective screening options include flexible sigmoidoscopy every 5 years, air-contrast barium enema every 5 years, and virtual colonoscopy every 5 years.
The colonoscope allows direct image transmission to a television screen and real-time visualization as the physician examines the large intestine. Smaller polyps may be removed entirely by a pair of forceps, whereas large ones may require more advanced techniques. Forceps may also be used for tissue sampling where tissue appears inflamed or for tumors that can't be surgically removed.
Other Diagnostic Methods for Colorectal Cancer
Stool tests are classified as diagnostic rather than screening for colorectal cancer. By the time stool tests become positive for tumor growth, the pathology has likely reached an advanced stage. Stool tests for occult blood, including FOBT (fecal occult blood testing) or FIT (fecal immunochemical testing) should be repeated annually. Stool tests for abnormal genes due to tumor cell shedding, should be repeated every 3 years.
While flexible sigmoidoscopy allows visualization of only the last third of the large intestine, it may detect 60% of all colorectal cancer.
Air-contrast barium enema allows visualization of tumor growth by instilling a mixture of radiopaque barium liquid and air into the colon from the rectum. Sensitivity for tumors is inferior to that of colonoscopy, achieving only a rate of 50% for growths that are 1 cm or larger.
Virtual colonoscopy is based on images that are captured by CT or MRI, creating pictures that resemble an actual colonoscopy. Sensitivity is 90% for polyps that exceed 1 cm in size, but is less than ideal for those that are smaller than 5 mm. Specificity can be impaired by fecal matter that could be mistaken as colonic polyps.
In addition to being the gold standard for colon cancer screening, colonoscopy is an essential follow-up tool when other screening or diagnostic methods yield abnormal results, including flexible sigmoidoscopy, air-contrast barium enema, virtual colonoscopy, and stool tests for either occult blood or mutated genes.
How to Prevent Colorectal Cancer?
The risks of colorectal cancer may be reduced by lifestyle modifications, including:
- High-fiber diet, including fruits and vegetables
- Restriction of red meat or high-fat diet
- Calcium and vitamin D supplements
- Routine physical exercise x 30 minutes 5 days a week
- Abstinence from tobacco and moderation in alcohol
- Weight control
In 2015, the World Health Organization declared that processed meat is carcinogenic, which includes sausage, ham, and deli meat. Even one sausage or 2 slices of bacon per day can increase the risk of colorectal cancer by 18%. Red meat, including beef, pork, and lamb, may also be carcinogenic. Such risks for cancer extend beyond the large intestine to include the pancreas and the prostate.
Smoking tobacco releases many chemicals which are carcinogenic to at least 18 organs that involve multiple systems, such as the ear, nose, and throat; digestive tract (esophagus, stomach, pancreas, liver, biliary tree, large intestine), urogenital system; and the respiratory tree.
Colorectal Cancer Screening is Essential Starting at Age 45
With screening, colorectal cancer is one of the most preventable cancers. Everyone ages 45 and older should undergo such screening. Besides being the most effective form of screening, colonoscopy is simple and safe. It potentially allows removal of all adenomas at the time of examination before they become malignant. Studies have shown that with the advent of colonoscopy, the incidence of colorectal cancer was reduced by two-thirds. Even if colorectal cancer is discovered, prompt colonoscopy will allow earlier diagnosis, thus conferring earlier staging, more effective treatment, and greater chance for cure.
We are grateful to Dr. and Mrs. Peter Fung for their generous support of this medical column.

