Did you know that November 12, 2019 is World Pneumonia Day? While you probably won’t be marking your calendar, the start of flu season is a good time to learn more about this serious lung infection.
When you have pneumonia, the tiny air sacs in the lungs fill up with fluid and pus. Breathing becomes more difficult and the body can’t take in as much oxygen. Pneumonia can range from a mild infection to a life-threatening condition requiring hospitalization.
Skip
Common Symptoms
Lobar pneumonia affects one or more of the lobes (sections) in one or both lungs. Bronchial pneumonia is found in patches throughout both lungs. Regardless of where the infection is concentrated, the symptoms are similar. The most common symptoms are a cough that produces green, yellow or bloody mucus, and a fever, often accompanied by shaking, chills and perspiring. Shortness of breath, rapid breathing and chest pain are also common. As the body is deprived of oxygen, a person may experience confusion and even delirium. The lips and fingernails may take on a bluish color.
There are different types of pneumonia, depending on what is causing the disease:
- Bacterial pneumonia. While several different types of bacteria can cause pneumonia, the infection is typically caused by streptococcus pneumoniae. This common bacterium also causes bronchitis, otitis media, septicemia and meningitis.
- Viral pneumonia. The flu (influenza) virus is the most frequent viral culprit, responsible for about one-third of all pneumonia cases. Once a person develops viral pneumonia, they are more vulnerable to bacterial pneumonia and may have to fight off both infections at once.
- Mycoplasma pneumonia. Often referred to as “atypical” or “walking” pneumonia, this milder type of pneumonia is caused by the mycoplasma pneumoniae bacteria. The most common symptoms are comparable to those of a chest cold — fatigue, sore throat, fever and coughing.
- Fungal pneumonia. Certain types of fungal infections can lead to pneumonia. In recent years, you may have read about “Valley Fever” affecting farm workers in the Central Valley. This is an example of a fungal infection that can lead to pneumonia.
Know the risk factors!
Pneumonia, especially the bacterial kind, can affect people of all ages. However, certain risk factors can increase your chance of developing the disease. These include:
- Being under the age of 4 or over 65
- Smoking
- Abusing alcohol
- COPD, asthma or chronic respiratory diseases
- Heart disease
- Recovering from a recent surgery
- A weakened immune system
- A current viral infection
- Diabetes
Treating Pneumonia
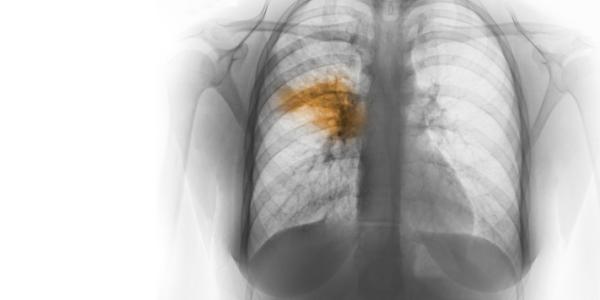
A variety of tests are used to diagnose a suspected case of pneumonia, including imaging of the lungs through an X-ray or CT. Your doctor may also order blood tests, bronchoscopy or a culture of coughed up phlegm.
Treatment depends on the type of pneumonia. Although severe cases may require hospitalization, pneumonia can usually be treated at home. Antibiotics are always used for bacterial pneumonia and can sometimes speed recovery from mycoplasma pneumonia. Most viral pneumonias get better on their own. Home treatment includes plenty of fluids, bed rest and medication to control the pain, fever and cough. While most people start to feel better within three to five days, the fatigue and cough may linger for weeks.
Preventing Pneumonia
Bacterial pneumonia is easily spread through coughing, sneezing and physical contact. That’s why it’s a good idea for certain groups to get vaccinated. Two vaccines help prevent pneumonia in people who are at-risk:
- PCV13 protects against 13 strains of pneumococcal bacteria
- PPSV23 protects against 23 strains of pneumococcal bacteria
Both vaccines provide protection against meningitis and bacteremia.
The Center for Disease Control (CDC) recommends PPSV23 for all adults aged 65 and older. That’s because pneumococcal pneumonia kills about one in 20 older adults who get it. If the pneumonia leads to bacteremia of meningitis, the odds are even worse — one in six older adults who develop either of these conditions will die. The vaccine is also recommended for adults 19 through 64 years old who smoke cigarettes or suffer from certain health conditions.
If you think you might be a candidate for a pneumonia vaccine, talk to your doctor. Just be aware that the CDC recommends against getting PCV13 and PPSV23 at the same time. If your doctor thinks you need both vaccines, get PCV13 first and schedule PPSV23 for another visit, as recommended by your healthcare professional.
Check with your insurance provider for details on whether there is any cost to you and for a list of in-network vaccine providers. Medicare Part B also covers 100% of the cost for both pneumococcal vaccines (when administered at least one year apart).
This article first appeared in the November 2019 edition of the HealthPerks newsletter.

